Fill Out Your Tb Test Template
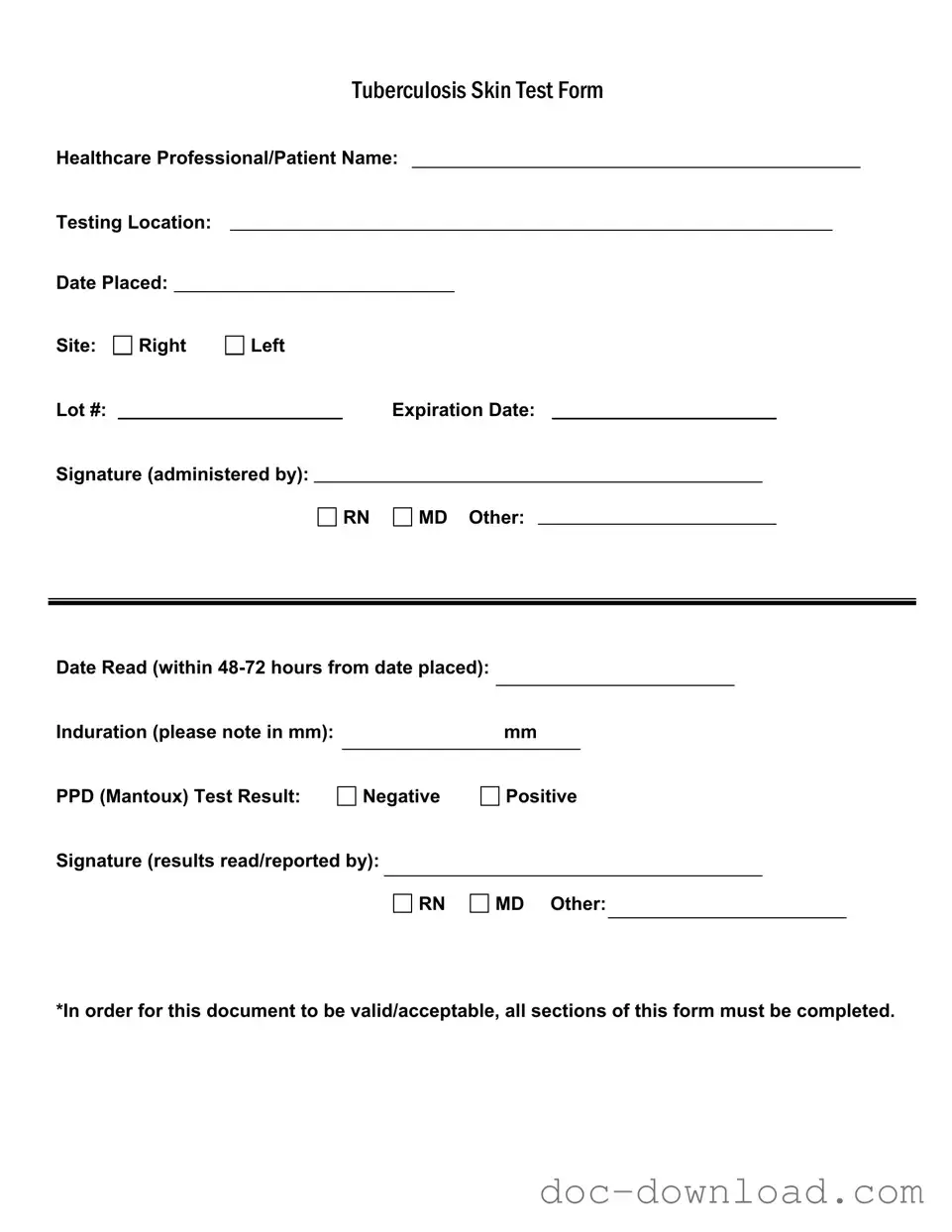
The Tuberculosis (TB) Skin Test form is an essential document used to record the details of a TB skin test, which is a common method for screening individuals for tuberculosis infection. This form captures critical information, including the names of both the healthcare professional administering the test and the patient receiving it, as well as the location where the test was performed. Key dates are also noted, such as the date the test was placed and the date it should be read, which is typically within 48 to 72 hours. The form requires the testing site to be specified, allowing for accurate tracking of results. Additionally, it includes a section for the lot number and expiration date of the test material, ensuring that the test is valid and reliable. After the test is read, the healthcare professional must record the induration measurement in millimeters, indicating whether the result is negative or positive. To maintain the integrity of the document, all sections must be filled out completely, and signatures from the administering professional and the person reading the results are required. This thorough documentation helps ensure proper follow-up and care for individuals tested for TB.
Similar forms
The Immunization Record form is similar to the TB Test form in that both documents serve as official records of health-related assessments. Each form requires the identification of the patient, the healthcare professional administering the test, and specific details regarding the procedure. Just as the TB Test form documents the results of a skin test, the Immunization Record tracks vaccinations received, including dates and types of immunizations. Completion of all sections is essential for both forms to be considered valid.
The Health Screening Questionnaire is another document akin to the TB Test form. This questionnaire gathers crucial health information from the patient, similar to how the TB Test form collects data about the test administered. Both documents require the patient’s name, the administering healthcare professional, and specific details about the assessment. Accurate completion is vital for both forms to ensure proper health evaluation and follow-up.
The Medical Clearance Form shares similarities with the TB Test form, particularly in its purpose of confirming an individual’s health status before participation in activities such as sports or employment. Both documents require signatures from healthcare professionals and detail the results of health assessments. Each form must be thoroughly completed to be deemed acceptable for its intended use.
The Laboratory Test Result form is comparable to the TB Test form as it provides documented evidence of specific health tests. Both forms include patient information, the name of the healthcare provider, and results of the tests conducted. The clarity and completeness of information on both documents are crucial for ensuring accurate interpretation and follow-up actions.
The Consent Form for Medical Procedures resembles the TB Test form in that both documents require patient identification and signatures from healthcare professionals. The Consent Form outlines the procedure being performed, while the TB Test form details the test conducted. Both documents must be filled out completely to ensure informed consent and compliance with healthcare regulations.
The Patient Health History form is similar to the TB Test form as it collects essential information about the patient’s medical background. Both forms require the patient’s name and details regarding their health status. The completeness of the Patient Health History form is critical, just like the TB Test form, to provide healthcare professionals with a comprehensive understanding of the patient’s health needs.
For individuals seeking to transfer property in Colorado, understanding the legal implications of a Quitclaim Deed is essential. This document can facilitate the process without the complexities typically associated with real estate transactions. If you're interested in obtaining a form to begin this process, visit quitclaimdocs.com/fillable-colorado-quitclaim-deed for a fillable version that ensures every detail is captured accurately.
The Referral Form for Specialist Consultation parallels the TB Test form in that both require patient identification and details regarding the healthcare provider. The Referral Form documents the reason for the referral, while the TB Test form records the test administered. Each form must be completed accurately to ensure that the patient receives the appropriate care and follow-up.
The Emergency Contact Form is similar to the TB Test form in its requirement for patient identification and relevant details. While the TB Test form documents health assessments, the Emergency Contact Form lists individuals who can be reached in case of an emergency. Both forms must be filled out completely to ensure that healthcare providers have access to necessary information when needed.
The Medication Administration Record is akin to the TB Test form as it serves as a log of treatments administered to a patient. Each document includes patient identification and details about the healthcare provider. The Medication Administration Record must be completed accurately to ensure proper tracking of medication, just as the TB Test form must be fully filled out to document test results.
The Physical Examination Report is comparable to the TB Test form, as both provide documentation of health evaluations. Each form includes patient information and details about the assessment performed. The Physical Examination Report encompasses a broader scope of health information, but like the TB Test form, it requires thorough completion to be valid and useful for ongoing patient care.
Form Specifications
| Fact Name | Description |
|---|---|
| Purpose | The Tuberculosis (TB) Test form is used to document the administration and results of the TB skin test, which is essential for detecting tuberculosis infection. |
| Healthcare Professional | The form requires the name of the healthcare professional administering the test, ensuring accountability and proper record-keeping. |
| Testing Location | It is important to include the testing location on the form, as this information may be relevant for follow-up and epidemiological purposes. |
| Induration Measurement | Induration, measured in millimeters (mm), is a critical component of the test result, indicating the presence or absence of a TB infection. |
| Result Interpretation | The form captures the test result as either negative or positive, which helps in determining the next steps for patient care. |
| Signature Requirement | Signatures from healthcare professionals are mandatory for both administering and reading the results, ensuring that the process is validated by qualified personnel. |
| Completion Requirement | All sections of the form must be completed for it to be valid and acceptable, underscoring the importance of thorough documentation. |
Different PDF Templates
Dnd 5e Character Sheet Fillable - Catchphrases or quotes your character is known for.
Minor Travel Consent Letter - This form may include details about potential risks associated with the activities for full parental awareness.
Utilizing the proper documentation is vital in real estate transactions, and for those engaging in property deals in Colorado, the Colorado Real Estate Purchase Agreement form serves as a cornerstone. This legally binding document delineates the terms governing the purchase or sale of real estate in the state, ensuring clarity and fairness. To assist in navigating this process successfully, you may find it helpful to refer to Colorado PDF Forms for access to essential templates and resources.
Facial Consent Forms - This form confirms that clients are free from any medical conditions prohibiting treatment.
Sample - Tb Test Form
|
|
|
|
|
TUBERCULOSISSKINTESTFORM |
||||||||
Healthcare Professional/Patient Name: |
|||||||||||||
Testing Location: |
|
|
|
|
|
|
|
|
|
|
|
||
Date Placed: |
|
|
|
|
|
|
|
|
|
|
|
|
|
Site: |
Right |
Left |
|
|
|
|
|
|
|
|
|||
Lot #: |
|
|
|
|
|
Expiration Date: |
|
|
|||||
Signature (administered by): |
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
RN |
|
MD Other: |
|
|
|
|||
Date Read (within |
|
|
|
|
|
|
|
Induration (please note in mm): |
|
mm |
|
PPD (Mantoux) Test Result: |
|
|
|
Negative |
Positive |
||
Signature (results read/reported by):
RN
MD Other:
*In order for this document to be valid/acceptable, all sections of this form must be completed.