Blank Do Not Resuscitate Order Document for Massachusetts
In Massachusetts, the Do Not Resuscitate (DNR) Order form plays a crucial role in respecting individuals' healthcare wishes, particularly at the end of life. This form is designed for patients who wish to decline cardiopulmonary resuscitation (CPR) and other life-saving measures in the event of cardiac or respiratory arrest. It is essential for patients to discuss their preferences with healthcare providers and family members before completing the form. The DNR Order must be signed by a physician, ensuring that it is recognized and honored by emergency medical services and healthcare facilities. Additionally, the form includes specific instructions regarding the patient's wishes, emphasizing the importance of clear communication and understanding. By having a DNR Order in place, individuals can maintain control over their medical care, ensuring that their preferences are respected during critical moments. This form not only reflects personal values but also alleviates the burden on family members and healthcare providers in making difficult decisions during stressful times.
Similar forms
The Massachusetts Do Not Resuscitate (DNR) Order form shares similarities with an Advance Healthcare Directive. Both documents are designed to communicate an individual's healthcare preferences when they are unable to express their wishes. An Advance Healthcare Directive typically encompasses a broader range of decisions, including preferences for medical treatments and appointing a healthcare proxy. While the DNR specifically addresses resuscitation efforts, the Advance Healthcare Directive provides a more comprehensive view of a person's desires regarding various medical interventions, ensuring that their values and choices are respected in critical situations.
Another document akin to the DNR is the Physician Orders for Life-Sustaining Treatment (POLST) form. Like the DNR, the POLST form is a medical order that outlines a patient's preferences for life-sustaining treatments. However, the POLST is more detailed, addressing not only resuscitation but also other interventions such as intubation and feeding tubes. Both documents require the signature of a healthcare provider, ensuring they are recognized and honored in medical settings. This allows patients to have their wishes followed, promoting dignity and respect in end-of-life care.
The Living Will is another important document that bears resemblance to the DNR Order. A Living Will specifies an individual's wishes regarding medical treatment in situations where they are terminally ill or incapacitated. While a DNR focuses solely on resuscitation efforts, a Living Will encompasses a wider array of medical decisions, such as the use of life support or pain management options. This document serves as a guide for healthcare providers and family members, helping them understand the patient's values and preferences during difficult times.
Similar to the DNR is the Healthcare Proxy form, which allows individuals to designate someone to make medical decisions on their behalf. While the DNR explicitly states preferences regarding resuscitation, the Healthcare Proxy empowers a trusted person to interpret and act upon the individual's wishes in various medical situations. This can include decisions about life-sustaining treatments, ensuring that the appointed proxy understands the patient's values and desires. Together, these documents create a comprehensive approach to managing healthcare decisions.
For those looking to mitigate risks during activities, a practical resource is the Release of Liability form for protective agreements, which serves as a critical tool in outlining responsibilities and minimizing potential claims.
Lastly, the Medical Power of Attorney (MPOA) is comparable to the DNR Order in that it grants authority to another person to make healthcare decisions for someone who is unable to do so. Like the Healthcare Proxy, the MPOA can address a range of medical issues, including resuscitation preferences. However, the MPOA is often broader in scope, allowing the appointed individual to make decisions about treatment options, hospitalization, and other healthcare matters. This document ensures that a person's healthcare choices are honored, even when they cannot communicate them directly.
Document Overview
| Fact Name | Details |
|---|---|
| Definition | A Do Not Resuscitate (DNR) Order instructs medical personnel not to perform cardiopulmonary resuscitation (CPR) if a patient's heart stops or they stop breathing. |
| Governing Law | The Massachusetts DNR Order is governed by Massachusetts General Laws Chapter 111, Section 70E. |
| Eligibility | Any adult who is capable of making medical decisions can complete a DNR Order. This includes individuals with terminal illnesses or severe health conditions. |
| Form Requirements | The DNR Order must be signed by the patient and a physician to be valid. It should also be clearly marked and easily accessible. |
| Revocation | A patient can revoke a DNR Order at any time. This can be done verbally or in writing, and it should be communicated to healthcare providers. |
| Emergency Medical Services | Emergency Medical Technicians (EMTs) must honor a valid DNR Order. They are trained to recognize and follow these orders in emergencies. |
| Placement | It is advisable to keep the DNR Order in a visible location, such as on the refrigerator or in a medical alert bracelet. |
| Patient Autonomy | The DNR Order supports patient autonomy by allowing individuals to make choices about their end-of-life care. |
| Communication | Discussing the DNR Order with family members and healthcare providers is essential to ensure everyone understands the patient's wishes. |
| Legal Status | A properly executed DNR Order is legally binding and must be respected by all healthcare providers in Massachusetts. |
Additional State-specific Do Not Resuscitate Order Forms
What Does a Dnr Look Like - A proactive approach to managing one’s healthcare wishes in emergencies.
A Colorado Quitclaim Deed is a legal document used to transfer ownership of real estate from one party to another without making any guarantees about the title's validity. This form is often utilized in situations such as transferring property between family members or clearing up title issues. For those looking to complete this process, fill out the form by clicking the button below, or visit quitclaimdeedtemplate.com/colorado-quitclaim-deed-template for more information.
Does a Dnr Need to Be Notarized in California - In many states, this order must comply with specific legal and procedural requirements to be valid.
Dnr and Dni Documents Are All Part of What Are Known as - Understanding how a DNR affects treatment can empower patients in their care journey.
Indiana Out of Hospital Dnr - Being informed about a DNR can alleviate anxiety for patients and their loved ones.
Sample - Massachusetts Do Not Resuscitate Order Form
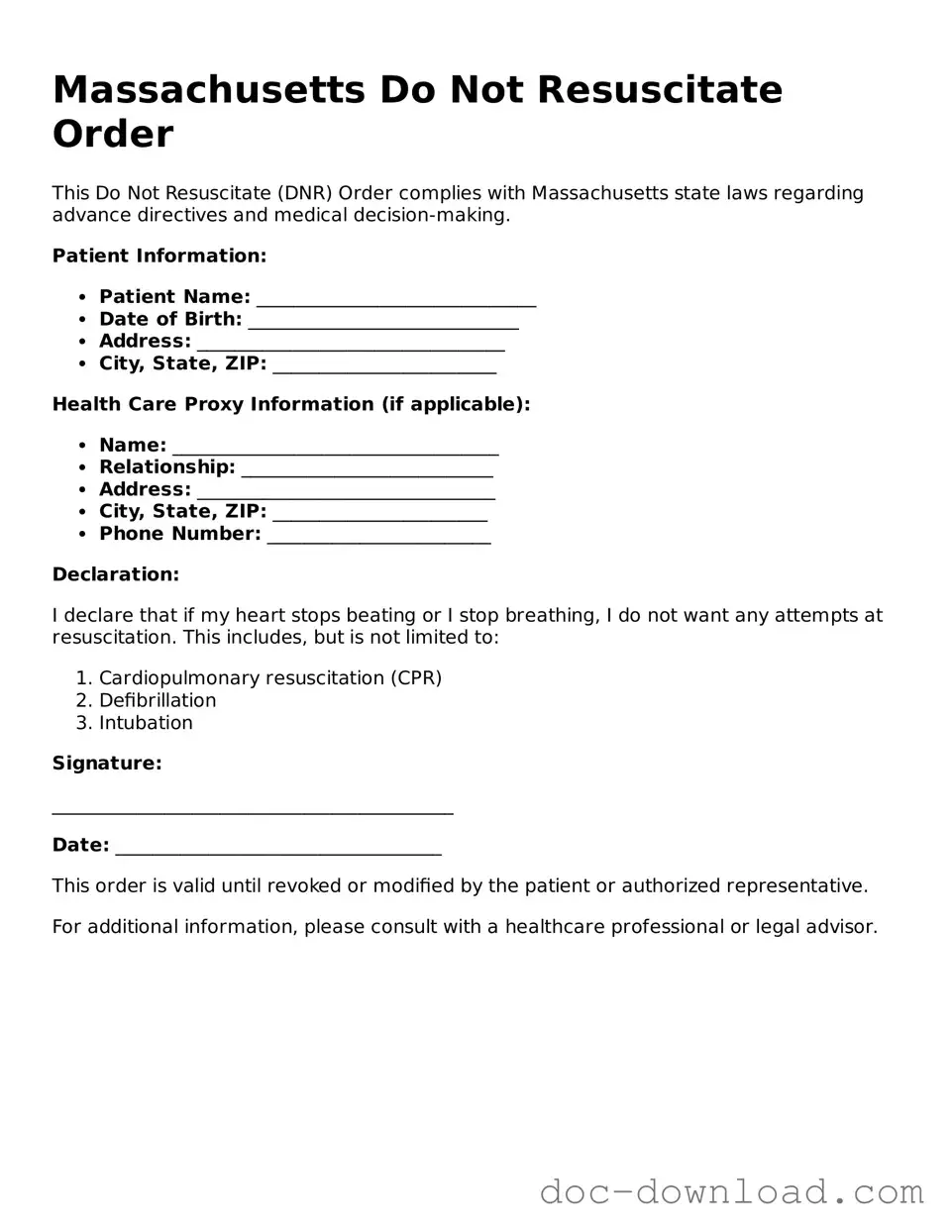
Massachusetts Do Not Resuscitate Order
This Do Not Resuscitate (DNR) Order complies with Massachusetts state laws regarding advance directives and medical decision-making.
Patient Information:
- Patient Name: ______________________________
- Date of Birth: _____________________________
- Address: _________________________________
- City, State, ZIP: ________________________
Health Care Proxy Information (if applicable):
- Name: ___________________________________
- Relationship: ___________________________
- Address: ________________________________
- City, State, ZIP: _______________________
- Phone Number: ________________________
Declaration:
I declare that if my heart stops beating or I stop breathing, I do not want any attempts at resuscitation. This includes, but is not limited to:
- Cardiopulmonary resuscitation (CPR)
- Defibrillation
- Intubation
Signature:
___________________________________________
Date: ___________________________________
This order is valid until revoked or modified by the patient or authorized representative.
For additional information, please consult with a healthcare professional or legal advisor.